Abstract

Background: Toxicities following allogeneic hematopoietic stem cell transplantation are specific to the conditioning regimen used and its intensity. Therefore, we hypothesized that the hazard of individual comorbidities is dependent on the conditioning agents and their dose. The aim of this analysis was to study, in a regimen specific manner, the impact of individual comorbidities (cardiac disease, severe pulmonary disease, and diabetes mellitus) on mortality.
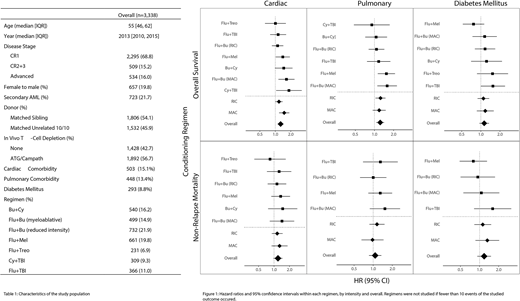
Methods: We included a multi-center cohort of 3,338 patients from the registry of the Acute Leukemia Working Party of the European Society of Blood and Marrow Transplantation (EBMT), who underwent first allogeneic HSCT for treatment of AML in all disease stages, transplanted between 2005 and 2016. Patients included received grafts from a matched sibling or 10/10 HLA-allele matched unrelated donor, and who were conditioned using one of 7 common regimens (Busulfan [BU[/Cyclophposphamide [Cy], Cy/Total Body Irradiation [TBI], Flu [Fludarabine]/Bu at reduced-intensity [RIC] dosage, Flu/Bu at myeloablative [MAC] dosage, Flu/Melphalan [Mel], Flu/Treosulfan [Treo], Flu/TBI). Regimens were excluded from a given analysis if fewer than ten overall mortality events occurred among patients with or without the studied condition. We constructed a multivariable Cox model for the outcome of overall survival, adjusted for key transplantation variables, including patient age, disease status, and donor type among others. For each comorbidity, separate models were constructed within each of the seven regimens, and the comorbidity's hazard ratio was extracted. Using the same method, the hazard ratio across all regimens, as well as in the myeloablative and the reduced-intensity setting, was obtained.
Results: The median age was 55 years; 70% of patients were in first complete remission (CR), and 54% of patients received grafts from matched sibling donors. The most common regimens studied were Flu/Bu at a reduced-intensity dose (22%), Flu/Mel (20%) and Bu/Cy (16%, Table 1). We find that the studied comorbidities were associated with different degrees of added risk for overall mortality in each regimen studied. For cardiac disease, hazard ratios (HR) ranged from 1.00 (95% CI: 0.63-1.60) in Flu/Treo to 1.65 (1.15-2.36) in Flu/Bu with myeloablative dose (Figure 1). Among patients with severe pulmonary disease, significant increases in hazard were seen only in patients treated with myeloablative Flu/Bu and Flu/Mel. In diabetes mellitus, no regimens were clearly associated with increased risk of overall mortality. However, Flu+TBI trended strongly toward increased risk with an HR of 1.55 (1.00-2.41, p = 0.051). Greater comorbidity-associated risk was not consistently associated with increasing conditioning, and the hazards associated with each comorbidity in the MAC and RIC settings were broadly overlapping. Similar trends were seen for the outcome of non-relapse mortality, although statistical significance (p < 0.05) was not observed in the setting of low event numbers.
Conclusions: These results confirm our hypothesis that comorbidities exert an effect on transplantation outcome in a conditioning regimen-specific manner. Additional study, both retrospective, and prospective, may eventually allow for the precision selection of a conditioning regimen based on the individual patient's physiological status.
Finke:Medac: Consultancy, Honoraria, Other: travel grants, Research Funding; Neovii: Consultancy, Honoraria, Other: travel grants, Research Funding; Riemser: Consultancy, Honoraria, Research Funding; Novartis: Consultancy, Honoraria, Other: travel grants, Research Funding. Malladi:Roche: Membership on an entity's Board of Directors or advisory committees. Mohty:MaaT Pharma: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal